Small bowel obstruction (SBO) is a significant medical condition that can lead to various complications if not treated promptly and effectively. Understanding the sequelae of a small bowel obstruction is crucial for both medical professionals and patients, as it helps in recognizing potential complications and implementing timely interventions. In this article, we will explore the long-term effects of SBO, highlighting the importance of early diagnosis and treatment to prevent adverse outcomes.
Small bowel obstruction can arise due to various causes, including adhesions, hernias, tumors, or inflammatory diseases. Regardless of the cause, SBO disrupts the normal flow of intestinal contents, leading to a buildup of pressure and potentially causing severe complications. The sequelae of a small bowel obstruction may include bowel ischemia, perforation, sepsis, and long-term digestive issues, all of which can significantly impact a patient's quality of life if not addressed promptly.
Effective management and understanding of the sequelae of a small bowel obstruction involve a multidisciplinary approach, combining medical, surgical, and supportive care. Recognizing the signs and symptoms early and seeking appropriate medical attention can help mitigate the risks associated with SBO. This comprehensive article aims to provide insights into the potential consequences of SBO, emphasizing the need for timely intervention and ongoing care to ensure optimal patient outcomes.
Read also:Voyager 1 The Marvel Of Human Ingenuity In Space Exploration
Table of Contents
- What is Small Bowel Obstruction?
- Causes of Small Bowel Obstruction
- Symptoms and Diagnosis
- Treatment Options
- How Does SBO Lead to Complications?
- Bowel Ischemia and Necrosis
- Perforation and Peritonitis
- Chronic Pain and Adhesions
- Nutritional Deficiencies
- Long-term Gastrointestinal Issues
- Psychological Impact of SBO
- Preventive Measures and Care
- Rehabilitation and Recovery
- Can SBO be Prevented?
- Frequently Asked Questions
- Conclusion
What is Small Bowel Obstruction?
A small bowel obstruction (SBO) occurs when there is a blockage in the small intestine that prevents the normal passage of food and liquids. This blockage can be partial or complete, causing a range of symptoms and potential complications. The small intestine is crucial for digestion and nutrient absorption, making any disruption in its function a serious concern.
The obstruction can result from various factors, such as adhesions from previous surgeries, hernias, tumors, or inflammatory diseases like Crohn's disease. When an obstruction occurs, it leads to a buildup of intestinal contents and gas, increasing pressure within the intestine. If not resolved, this pressure can compromise blood flow, leading to ischemia and, eventually, tissue death.
SBO is a common condition requiring immediate medical attention to prevent severe complications. Timely diagnosis and treatment are essential to restore normal intestinal function and prevent long-term sequelae. A comprehensive understanding of the causes and symptoms of SBO is critical for effective management and improved patient outcomes.
Causes of Small Bowel Obstruction
Small bowel obstruction can arise from several underlying causes, each contributing to the development of this condition in different ways. The most common causes include:
- Adhesions: Bands of scar tissue that form after abdominal surgeries, causing the intestines to stick together and leading to blockage.
- Hernias: Protrusions of intestinal tissue through a weak spot in the abdominal wall, which can trap and obstruct the bowel.
- Tumors: Growths within the intestine that can block the passage of food and liquids.
- Inflammatory Bowel Diseases: Conditions like Crohn's disease can cause inflammation and narrowing of the intestinal passage.
- Intussusception: A condition where a part of the intestine slides into an adjacent section, often seen in children.
- Volvulus: Twisting of the intestine, cutting off blood supply and causing obstruction.
Each of these causes requires specific diagnostic approaches and treatment strategies to effectively manage the obstruction and prevent further complications. Understanding the underlying cause is key to tailoring the appropriate intervention and minimizing the risk of recurrence.
Symptoms and Diagnosis
The symptoms of small bowel obstruction can vary depending on the severity and location of the blockage. Common symptoms include:
Read also:Unveiling The Secrets Of Tai B52 A Comprehensive Guide
- Abdominal pain and cramping
- Nausea and vomiting
- Bloating and distension
- Inability to pass gas or stool
- Dehydration
- Fever and rapid heart rate (in severe cases)
Early diagnosis of SBO is crucial to prevent complications. Healthcare professionals use a combination of physical examination, imaging studies, and laboratory tests to diagnose the condition. Common diagnostic tools include:
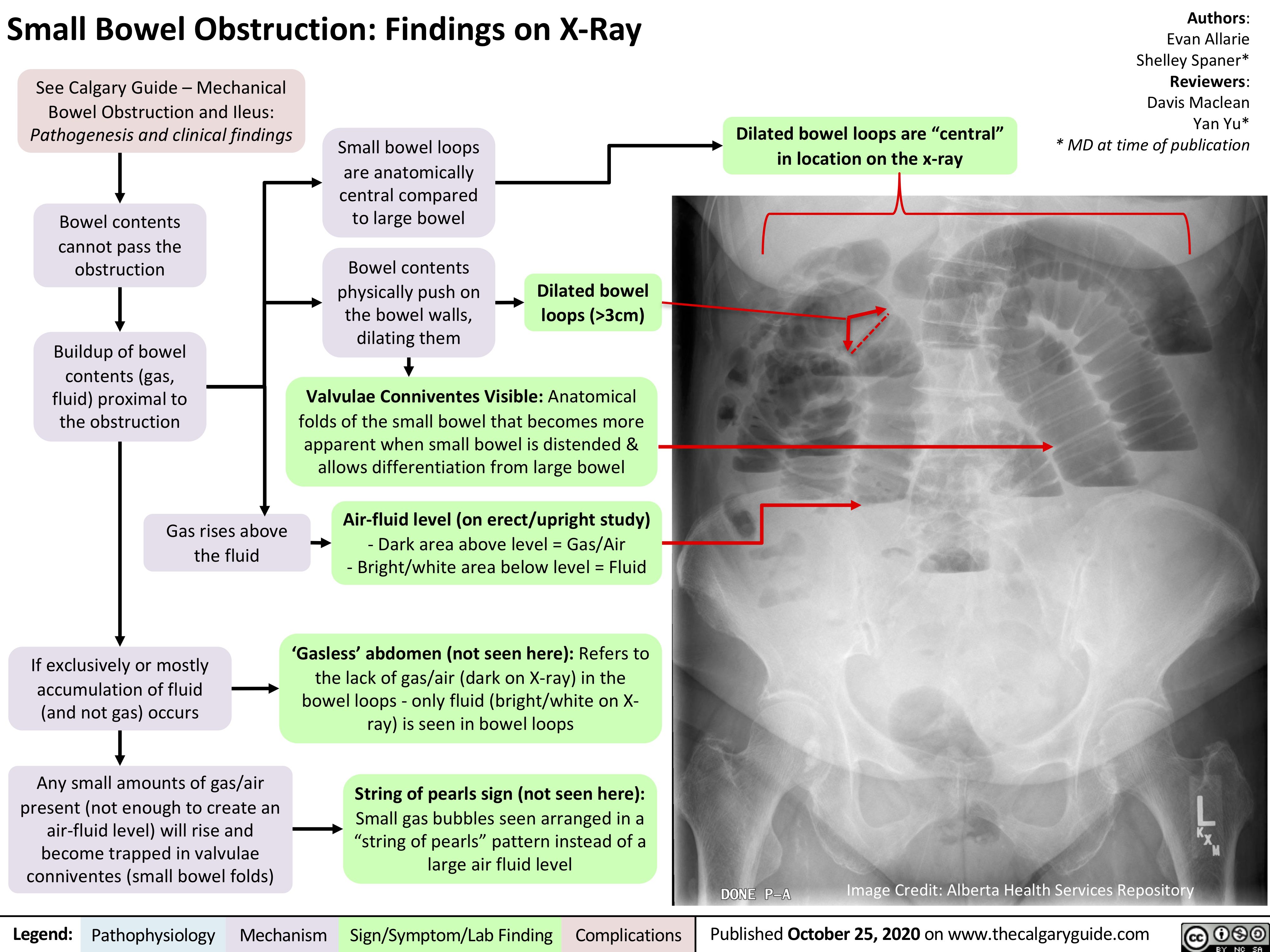
- Abdominal X-rays: To identify air-fluid levels and dilated bowel loops indicative of obstruction.
- CT Scans: Provide detailed images of the abdomen, helping to determine the location and cause of the obstruction.
- Ultrasound: Useful in children or pregnant women to avoid radiation exposure.
- Blood Tests: To assess electrolyte imbalances and signs of infection or inflammation.
Accurate diagnosis guides the treatment plan, allowing for timely intervention and reducing the risk of sequelae associated with SBO.
Treatment Options
The treatment of small bowel obstruction depends on the cause, severity, and location of the blockage. Treatment strategies aim to relieve the obstruction, restore normal bowel function, and prevent complications. Common treatment options include:
- Conservative Management: Includes bowel rest, intravenous fluids, and nasogastric tube insertion to relieve pressure and decompress the bowel. This approach is often used for partial obstructions.
- Surgical Intervention: Required for complete obstructions, strangulated bowel, or when conservative measures fail. Surgery may involve removing the obstructed segment, releasing adhesions, or repairing hernias.
- Endoscopic Procedures: Useful for removing certain types of blockages, such as bezoars or foreign bodies, without invasive surgery.
- Medications: In some cases, medications may be used to manage symptoms or underlying conditions contributing to the obstruction, such as anti-inflammatory drugs for Crohn's disease.
Timely and appropriate treatment is essential to prevent sequelae of a small bowel obstruction, ensuring a swift recovery and reducing the risk of long-term complications.
How Does SBO Lead to Complications?
Small bowel obstruction can lead to complications when the blockage results in increased pressure within the intestine, compromising blood flow and leading to tissue damage. The following mechanisms contribute to the development of complications:
- Increased Intraluminal Pressure: Causes edema and impairs venous return, leading to ischemia and potential necrosis of the bowel tissue.
- Compromised Blood Supply: Severe obstruction can cut off blood flow, resulting in bowel ischemia and necrosis.
- Bacterial Translocation: Obstruction can allow bacteria to cross the intestinal barrier, leading to infection and sepsis.
- Perforation Risk: Prolonged pressure can weaken the bowel wall, increasing the risk of perforation and subsequent peritonitis.
Understanding these mechanisms is crucial for healthcare professionals to anticipate and promptly address potential complications, minimizing the risk of sequelae and improving patient outcomes.
Bowel Ischemia and Necrosis
Bowel ischemia occurs when the blood supply to a segment of the intestine is reduced or blocked, leading to oxygen deprivation and tissue damage. In the context of small bowel obstruction, increased pressure within the intestine can compromise blood flow, resulting in ischemia. If left untreated, ischemia can progress to necrosis, where the tissue dies and loses function.
The signs of bowel ischemia and necrosis may include severe abdominal pain, fever, elevated white blood cell count, and metabolic acidosis. Prompt recognition and intervention are crucial to prevent irreversible damage and life-threatening complications.
Treatment of bowel ischemia often requires surgical intervention to remove the affected segment and restore blood flow. Early diagnosis and treatment are essential to prevent sequelae of a small bowel obstruction, such as bowel necrosis and sepsis.
Perforation and Peritonitis
Perforation is a serious complication of small bowel obstruction where a hole forms in the bowel wall, allowing its contents to leak into the abdominal cavity. This can lead to peritonitis, a severe and potentially life-threatening inflammation of the peritoneum, the lining of the abdominal cavity.
Signs and symptoms of perforation and peritonitis include sudden, severe abdominal pain, fever, tachycardia, and signs of sepsis. Immediate medical intervention is required to address these complications, typically involving surgical repair of the perforation and antibiotic therapy to treat infection.
Preventing perforation and peritonitis requires early detection and treatment of small bowel obstruction. Recognizing the signs of impending perforation is crucial for healthcare providers to initiate timely surgical intervention and prevent sequelae of a small bowel obstruction.
Chronic Pain and Adhesions
Chronic pain and adhesions are common sequelae of a small bowel obstruction, particularly following surgical intervention. Adhesions are bands of scar tissue that form between abdominal tissues and organs, often as a result of surgery. These adhesions can cause chronic pain, bowel obstruction, and difficulty with digestion.
Chronic pain resulting from adhesions can significantly impact a patient's quality of life, leading to physical and emotional distress. Management of chronic pain may involve physical therapy, pain medications, and, in some cases, surgical intervention to release the adhesions.
Preventing adhesions and managing chronic pain require a multidisciplinary approach, focusing on minimizing surgical trauma and employing techniques to reduce adhesion formation during surgery. Early recognition and treatment of chronic pain are essential to improve patient outcomes and prevent long-term sequelae of a small bowel obstruction.
Nutritional Deficiencies
Nutritional deficiencies are a potential sequelae of a small bowel obstruction, particularly in cases of prolonged obstruction or surgical resection of the intestine. The small intestine plays a vital role in nutrient absorption, and any disruption in its function can lead to malabsorption and deficiencies in essential vitamins and minerals.
Common nutritional deficiencies associated with small bowel obstruction may include:
- Vitamins: Deficiencies in vitamins A, D, E, and K due to malabsorption of fat-soluble vitamins.
- Minerals: Calcium, iron, and magnesium deficiencies due to impaired absorption in the small intestine.
- Protein: Inadequate protein intake and absorption can lead to muscle wasting and weakness.
Managing nutritional deficiencies involves dietary modifications, supplementation, and, in some cases, enteral or parenteral nutrition support. Early recognition and treatment of nutritional deficiencies are crucial to prevent long-term sequelae and improve overall health and well-being.
Long-term Gastrointestinal Issues
Long-term gastrointestinal issues are a potential sequelae of a small bowel obstruction, impacting a patient's quality of life and overall health. These issues may include altered bowel habits, ongoing pain or discomfort, and digestive problems.
Common long-term gastrointestinal issues associated with small bowel obstruction include:
- Altered Bowel Habits: Changes in bowel movements, such as diarrhea or constipation, can persist after resolution of the obstruction.
- Abdominal Pain and Discomfort: Chronic pain or discomfort may result from adhesions or other complications.
- Digestive Problems: Difficulty digesting certain foods or maintaining a balanced diet due to malabsorption or altered intestinal function.
Managing long-term gastrointestinal issues involves a comprehensive approach, including dietary modifications, medications to manage symptoms, and regular follow-up with healthcare providers. Early recognition and intervention are essential to prevent sequelae of a small bowel obstruction and improve patient outcomes.
Psychological Impact of SBO
The psychological impact of small bowel obstruction is an often-overlooked sequelae, affecting a patient's mental health and well-being. The experience of a medical emergency, hospitalization, and potential long-term complications can lead to anxiety, depression, and stress.
Common psychological impacts of small bowel obstruction include:
- Anxiety and Stress: Concerns about health, treatment, and potential complications can cause significant stress and anxiety.
- Depression: The impact of chronic pain, dietary restrictions, and lifestyle changes can contribute to feelings of depression.
- Emotional Distress: Coping with a medical condition and its sequelae can lead to emotional distress and affect relationships.
Addressing the psychological impact of small bowel obstruction requires a holistic approach, incorporating mental health support, counseling, and stress management techniques. Early recognition and intervention are crucial to prevent sequelae of a small bowel obstruction and improve overall well-being.
Preventive Measures and Care
Preventive measures and care are essential to mitigate the risk of sequelae of a small bowel obstruction and improve patient outcomes. These measures focus on early detection, timely intervention, and ongoing management to prevent complications and recurrence.
Preventive measures and care strategies include:
- Regular Monitoring: Routine follow-up with healthcare providers to monitor for signs of obstruction and manage underlying conditions.
- Dietary Modifications: Adopting a balanced diet rich in fiber to promote healthy digestion and prevent constipation.
- Lifestyle Adjustments: Maintaining a healthy weight, avoiding heavy lifting, and managing stress to reduce the risk of recurrence.
- Adhesion Prevention: Employing surgical techniques and medications to minimize adhesion formation during surgical procedures.
Preventive measures and care are crucial to prevent sequelae of a small bowel obstruction, ensuring optimal health and quality of life for affected individuals.
Rehabilitation and Recovery
Rehabilitation and recovery are critical components of managing the sequelae of a small bowel obstruction. A comprehensive rehabilitation plan focuses on restoring normal function, improving quality of life, and preventing recurrence.
Key elements of rehabilitation and recovery include:
- Physical Therapy: Exercises and activities to improve strength, mobility, and overall fitness.
- Nutritional Support: Dietary counseling and supplementation to address nutritional deficiencies and promote a balanced diet.
- Pain Management: Medications and therapies to manage chronic pain and improve comfort.
- Psychological Support: Counseling and mental health services to address emotional distress and improve well-being.
Rehabilitation and recovery are essential to prevent sequelae of a small bowel obstruction, promoting long-term health and well-being for affected individuals.
Can SBO be Prevented?
While it may not be possible to prevent all cases of small bowel obstruction, certain measures can reduce the risk of developing this condition and its sequelae. Prevention focuses on lifestyle modifications, early detection, and managing underlying conditions.
Strategies to prevent small bowel obstruction include:
- Healthy Lifestyle: Maintaining a balanced diet, regular exercise, and a healthy weight to promote optimal digestion and reduce the risk of obstruction.
- Avoiding Adhesions: Minimizing surgical interventions when possible and using adhesion-prevention techniques during surgery.
- Managing Underlying Conditions: Regular monitoring and treatment of conditions like Crohn's disease or hernias to prevent complications.
- Early Detection: Recognizing and addressing symptoms of obstruction promptly to prevent progression and complications.
Implementing preventive measures can reduce the risk of small bowel obstruction and its sequelae, improving overall health and quality of life for individuals at risk.
Frequently Asked Questions
1. What are the early signs of a small bowel obstruction?
Early signs of a small bowel obstruction include abdominal pain and cramping, nausea, vomiting, bloating, and an inability to pass gas or stool.
2. How is small bowel obstruction diagnosed?
Small bowel obstruction is diagnosed using a combination of physical examination, imaging studies (such as X-rays or CT scans), and laboratory tests to assess electrolyte imbalances and signs of infection.
3. What are the treatment options for small bowel obstruction?
Treatment options for small bowel obstruction include conservative management (bowel rest, IV fluids), surgical intervention, endoscopic procedures, and medications to manage symptoms or underlying conditions.
4. Can small bowel obstruction lead to long-term complications?
Yes, small bowel obstruction can lead to long-term complications such as bowel ischemia, perforation, chronic pain, adhesions, nutritional deficiencies, and psychological impacts if not treated promptly and effectively.
5. How can nutritional deficiencies be managed after a small bowel obstruction?
Managing nutritional deficiencies involves dietary modifications, supplementation, and, in some cases, enteral or parenteral nutrition support to ensure adequate intake of essential vitamins and minerals.
6. Is there a way to prevent small bowel obstruction?
While not all cases can be prevented, strategies such as maintaining a healthy lifestyle, avoiding adhesions, managing underlying conditions, and early detection can reduce the risk of small bowel obstruction and its sequelae.
Conclusion
Understanding the sequelae of a small bowel obstruction is vital for effective management and prevention of complications. Early recognition and intervention are key to mitigating the risks associated with SBO, ensuring optimal patient outcomes. By implementing preventive measures, managing underlying conditions, and providing comprehensive rehabilitation and recovery support, healthcare providers can improve the quality of life for individuals affected by SBO. Continued research and education are essential to enhance our understanding and management of this complex condition, ultimately leading to better patient care and outcomes.
For more information on the sequelae of a small bowel obstruction, visit Mayo Clinic.